Nursing home residents are among the most vulnerable to COVID-19.
Although they account for less than 2 percent of the nation’s total COVID cases, they make up 20 percent of total deaths due to COVID.
In total, more than 137,000 nursing home residents have died from the virus in the U.S.
Perhaps because of this, just under 90 percent of Wisconsin nursing home residents have been vaccinated against COVID, a rate higher than any other demographic in the state.
However, staff members at nursing homes are not getting vaccinated at similar rates.
Statewide, 63 percent of nursing home staff members have been vaccinated against the coronavirus.
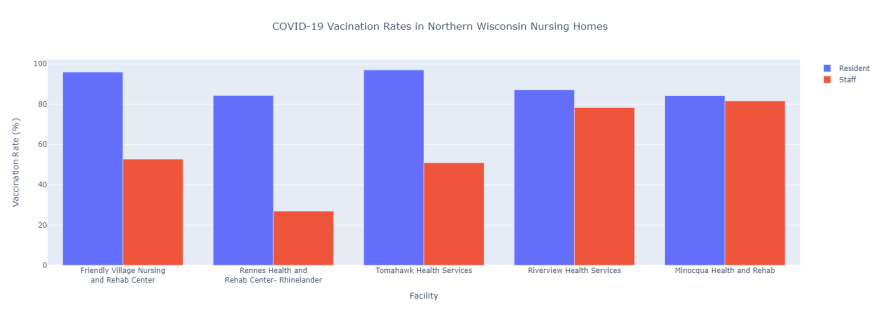
There is a gap between patient and staff vaccination rates at Wisconsin’s nursing homes, and that gap widens when looking at data from some local nursing homes.
For example, at Rennes Health and Rehab Center in Rhinelander about 84 percent of patients are vaccinated against COVID, according to data compiled by the Centers for Medicare and Medicaid Services.
However, the vaccine rate among staff members is 27 percent.
The gap at Rhinelander’s Friendly Village Nursing and Rehab Center is only slightly narrower.
While 96 percent of its residents are vaccinated, about 50 percent of its staff can say the same.
Neither facility responded to a request for comment from WXPR, but a representative from AARP did.
“I’m a little appalled by the fact that people in nursing homes are older and sicker, and here we have people who say they’re health care providers, and they’re kind of writing people off, like ‘these people are vulnerable but so what?’” says Helen Marks Dicks, the state issues advocacy director for AARP Wisconsin.
Marks Dicks says unvaccinated nursing home staff members risk bringing COVID into an environment where people are most at risk, and that could come at a deadly cost.
But that is not the only reason she argues staff members should get vaccinated.
“Even if they don’t bring in the disease, what they do is they end up sending people into quarantine because they themselves test positive,” she says. “That only puts all those people who are already socially isolated back into quarantine and isolation, and it prevents visitation from families.”
Because of this, Marks Dicks thinks a vaccine mandate for health care workers is not just a viable solution, but a good one.
“Which is worse,” she questions, “losing a staff person to a positive COVID or losing them because they didn’t get vaccinated? Either way, chances are they aren’t going to be working.”
Not everyone shares this perspective, however.
Rick Abrams, the CEO of the Wisconsin Health Care Association and the Wisconsin Center for Assisted Living, worries that a sweeping vaccine mandate will cause nursing homes that are already short-staffed to lose critical employees.
“The number one priority of any health care provider of any health care facility is to care for the residents and ensure that they are in the safest, highest quality environment,” Abrams says. “So having employees, albeit unvaccinated, there to care for our residents is the number one priority, followed closely by trying to get as many of our employees as possible vaccinated.”
Vaccine mandates have shown to motivate people to get vaccinated in recent weeks.
United Airlines, for example, implemented a mandate in early August. Now, the company claims 99.5 percent of its employees have gotten the COVID shot.
But Abrams says the situation in Wisconsin’s nursing homes is more dire.
“Our situation is that we can’t afford to lose one employee from our facilities,” he says.
He worries a mandate will cause that to happen.
“The mandate for health care workers only applies to facilities that receive Medicare or Medicaid funding,” he explains. “In addition — and this is probably the worst possible outcome — we’re going to see people leave the sector, and when I say the sector, not only long-term care, but health care generally.”
Abrams expects a federal vaccine mandate will go into effect sometime between the middle and end of October.
Until then, nursing homes in the Northwoods are left to grapple with two crises, a global pandemic and a serious staffing shortage.
Will trying to solve one worsen the other?






