With this latest Delta surge of COVID-19, overall hospitalizations have been lower than what the North Central Region experienced last fall and winter.
But the hospitals are experiencing much higher rates of patients that end up in the intensive care unit.
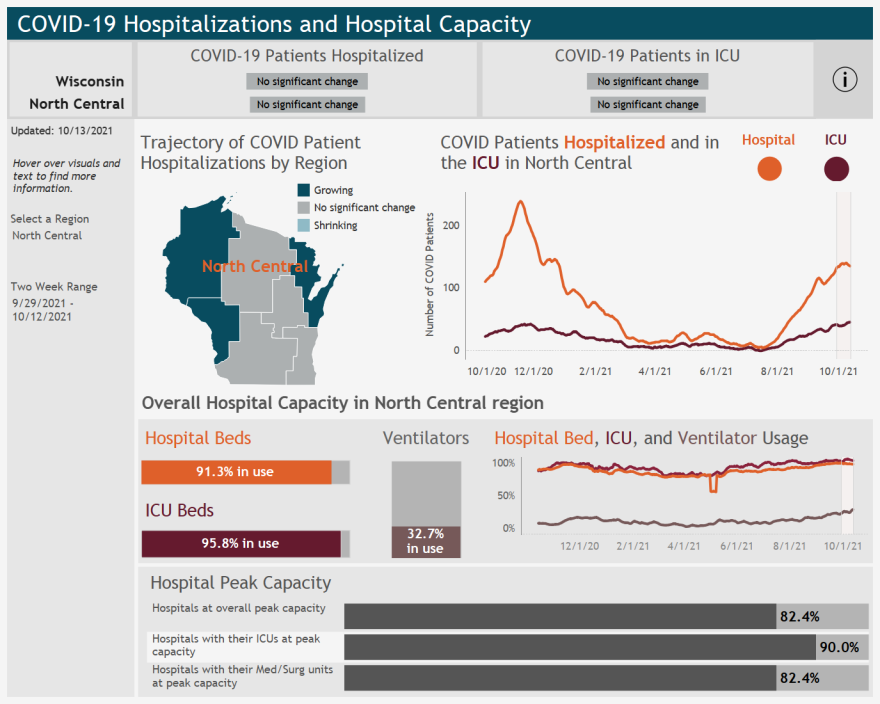
For a month now, there’s never been fewer than 35 ICU COVID patients on any given day in the region, with the highest be 50 ICU patients.
For comparison, in June and July when cases were at their lowest in the past year, there were weeks of just one or two patients in the ICU.
Ann Zenk is the Senior Vice President of Workforce and Clinical Practice for the Wisconsin Hospital Association.
She said while the surge last fall had a higher number of hospitalizations, it hit different regions at different times.
“This surge is statewide. It’s occurring in every region, pretty much at the same time. Hospitals and regions really can’t help each other out as much as they did during the surge last fall,” said Zenk.
Other differences with this surge are hospitals are seeing younger patients hospitalized.
And more patients are ending up in the ICU.
She said the high number of ICU COVID patients throughout the state is putting a strain on a pre-pandemic problem: a shrinking workforce.

“It takes a higher number of nurses and respiratory therapists, physicians and other specialists working to take care of ICU patients,” said Zenk.
The before the pandemic, Wisconsin’s workforce was already aging towards retirement, with not enough people to fill their positions.
This issue is not unique to the healthcare industry, but Zenk says it creates more complications for hospitals and clinic.
“It’s a double whammy for healthcare because not only are we seeing faster retirement, but older people create greater healthcare demand. We’re getting it on both fronts,” she said.
Zenk says if you need emergency care, for COVID or otherwise, you’ll experience longer wait times or may be sent to another hospital.
Though she stresses that if you are feeling sick, seek appropriate care.
“Go to the emergency room if you have to. We’re hearing from some of our members that folks with COVID are arriving sicker than they had previously experienced,” she said.
Zenk said the best way to relieve the stress on our hospital systems is to prevent the spread of illness.
This means washing your hands, staying home if you’re sick, and getting vaccinated if you haven’t already.
“Both the flu, cause we’re entering into influenza season, and COVID-19 vaccinations really do help limit the spread of severity of illness and reduce hospitalizations,” said Zenk.
DHS data for the month of September shows unvaccinated people are 9 times more like to be hospitalized if they get COVID as compared to vaccinated people.
You are 19 times more like to die from COVID if you’re unvaccinated.



